PECs Nerve Block
Evolving Approaches to Analgesia in Anterior Chest Wall and Breast Reconstruction Procedures
Until recently, regional anesthetic options for patients undergoing anterior chest wall procedures involving the pectoral muscles—such as breast reconstruction—were limited to thoracic epidural and thoracic paravertebral blocks (PVB). Given the increasing trend toward outpatient surgical care, the use of thoracic epidurals has become less favorable due to logistical challenges and the potential for significant complications.
The thoracic paravertebral block has emerged as a more commonly employed alternative for these cases. While it offers a favorable safety profile and longer duration of action, its efficacy in providing adequate analgesia for reconstructive breast surgery is often suboptimal. A key limitation lies in its inability to adequately address pain originating from the pectoral musculature.
This is particularly relevant in procedures where breast implants are placed in a subpectoral position—a common surgical practice. In such cases, patients frequently report significant discomfort related to pectoral muscle tension, spasm, and pressure, both in the immediate postoperative period and during recovery. The primary source of pain is muscular, rather than dermal, fascial, or glandular, and thus falls outside the effective territory of thoracic PVBs.
This mismatch between the innervation targeted by the paravertebral block and the actual pain generators in reconstructive breast procedures highlights the need for more anatomically appropriate regional techniques. The likely explanation for the ineffectiveness of the PVB in these cases is that the pectoral muscles are not innervated by the spinal afferents that travel in the intercostal spaces, which are the primary targets of the thoracic paravertebral block.
Pectoral Nerve Blocks for Breast Reconstruction: A Novel Regional Technique
A newer regional anesthesia technique has recently gained attention for its potential to improve analgesia in breast reconstruction procedures by specifically targeting the innervation of the pectoral muscles. Known as medial and lateral pectoral nerve blocks, this approach is simple, effective, and considered to have a favorable safety profile. Although still relatively novel and not yet extensively studied, early clinical use suggests significant promise.
This technique leverages the superficial location of the target nerves and does not require direct visualization of the nerves themselves. Given that the pectoral muscles are superficial and easily imaged with even lower-resolution ultrasound equipment, the block is accessible and practical in a wide range of clinical settings.
Anatomical Basis
The medial pectoral nerve originates from the medial cord of the brachial plexus, receiving contributions from C8–T1. After branching from the plexus, it travels through the fascial plane between the pectoralis major and pectoralis minor muscles, giving off several branches that penetrate and innervate the pectoralis major.
The lateral pectoral nerve arises from the lateral cord of the brachial plexus and receives contributions from C5–C7. Like the medial pectoral nerve, it travels in the same fascial plane between the pectoralis major and minor muscles, but its innervation is limited exclusively to the pectoralis major.
The shared anatomical plane between these two muscles—commonly referred to as the pectoralis (PECS) plane—serves as the target for this block. By depositing local anesthetic within this interfascial space, both the medial and lateral pectoral nerves can be effectively anesthetized, offering targeted relief from the muscular pain that commonly follows reconstructive breast surgery.
Medial and Lateral Pectoral Nerve Block: Technique and Considerations
The safe and effective performance of any peripheral nerve block begins with appropriate patient and procedural selection, thorough informed consent including a discussion of risks and benefits, and adherence to institutional protocols for laterality verification and time-out procedures.
Contraindications include:
Patient refusal
Infection at the planned injection site
Allergy to local anesthetics
Caution is advised in patients with anticoagulation, as the risk of hematoma or bleeding is increased.
Overview of the Pectoral Nerve Block Technique
The medial and lateral pectoral nerve block is performed as an ultrasound-guided hydrodissection within the fascial plane between the pectoralis major and pectoralis minor muscles, targeting the anatomical course of the respective nerves. This approach is sometimes referred to as the PECS I block.
Preparation and Patient Positioning
Confirm the correct side for the block.
Position yourself contralateral to the block side.
Apply standard ASA monitors and provide light sedation as appropriate.
Place the ultrasound machine on the same side as the block to maintain ergonomic alignment and visual control.
Use a high-frequency linear probe, typically set to a depth of 2–4 cm. In muscular patients, adjust the depth accordingly to accommodate larger pectoral muscle mass.
Ultrasound Anatomy and Imaging
Position the probe just inferior to the clavicle, similar to an infraclavicular brachial plexus approach.
Optimize the image to visualize the pectoralis major superficially and the pectoralis minor deep to it, both in short axis.
Identify nearby structures such as the thoracoacromial artery and subclavian/axillary vessels.
Rotate the probe into long axis orientation to facilitate needle guidance away from the chest wall, reducing risk of pleural puncture.
Block Execution
Administer skin anesthesia using a small needle (e.g., 25G) in awake patients.
Advance a blunt-tipped block needle in-plane, toward the fascial plane between the two pectoral muscles.
Use dynamic imaging to assist localization—for example, gently moving the patient’s elbow may cause the pectoralis muscles to move independently, accentuating the fascial plane.
Upon negative aspiration, hydrodissect the plane with local anesthetic to ensure adequate spread along the nerve course. Avoid injecting directly into the muscle bellies, as this may result in reduced efficacy and more rapid systemic absorption.
Typical volumes are 10 mL of local anesthetic, although further studies are needed to establish optimal dosing. Following successful hydrodissection, a perineural catheter may be placed for continuous infusion, taking care to avoid the surgical field.
Dosing Considerations and Combined Techniques
When used in conjunction with a thoracic paravertebral block, reduced dosing is recommended to avoid exceeding toxic thresholds—especially important in thin patients undergoing bilateral mastectomy and reconstruction. For these cases, consider omitting a bolus dose in the pectoral plane and instead initiating a slow infusion (e.g., 5 mL/hour) via catheter on each side. Tailoring the technique and dosing to the surgical plan and patient body habitus is essential for both efficacy and safety.
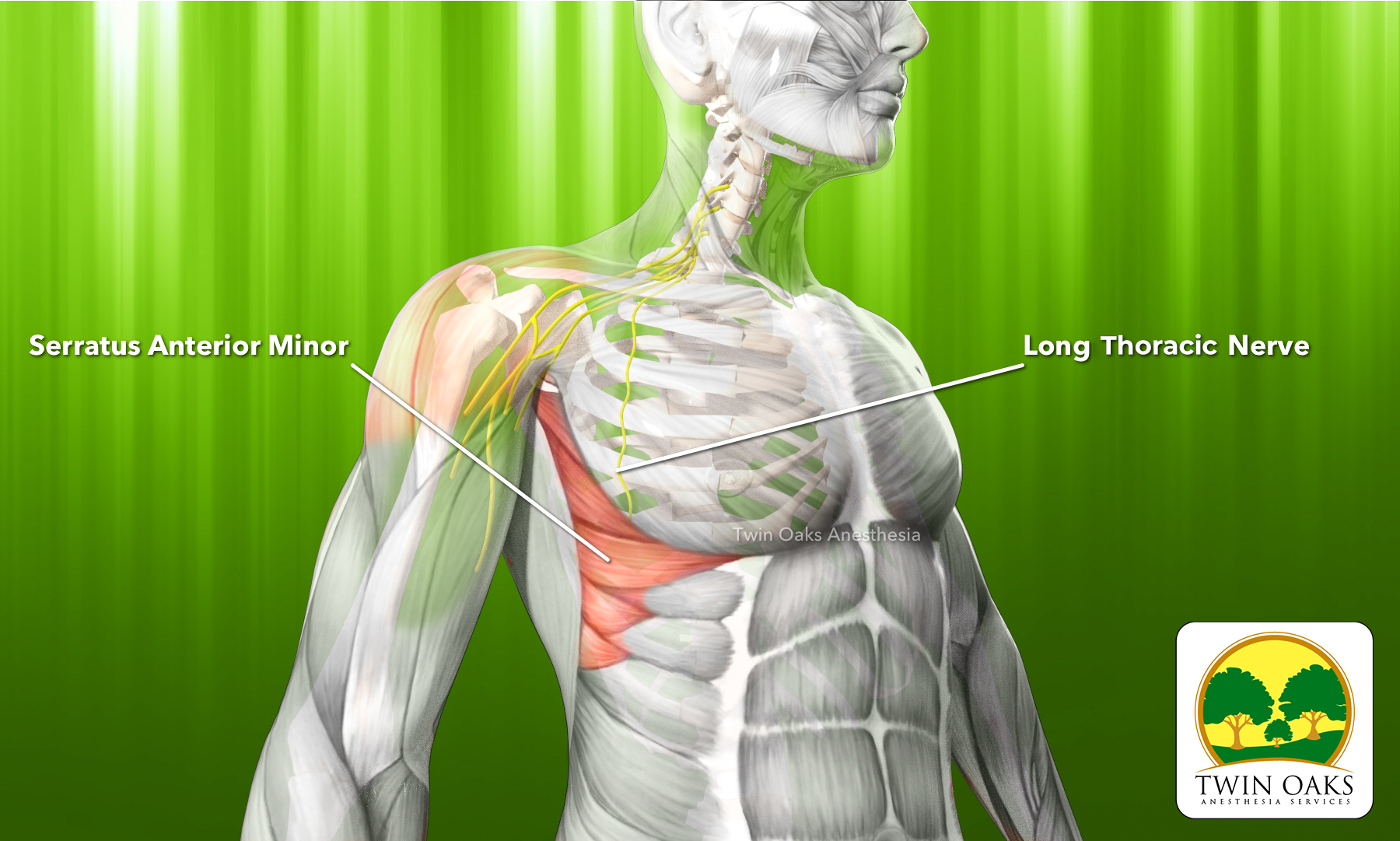
Image Reference:
The image below illustrates the relevant anatomy for the PECS I block, with the pectoralis major visualized superficially, pectoralis minor deep to it, and the thoracoacromial artery traversing the interfascial plane.
These procedure notes are intended as a foundational reference to support and streamline your documentation. You are encouraged to adapt them to align with your institution’s policies. Please note: they are not intended for unmodified use, and we assume no liability for procedural outcomes or alterations made to the content.